Losartan and its active metabolite block the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT₁ receptor in various tissues, such as vascular smooth muscle and the adrenal gland. Both losartan and its principal metabolite have a much greater affinity (about 1000-fold) for the AT₁ receptor than for the AT₂ receptor.
Hydrochlorothiazide is a thiazide diuretic that affects renal tubular mechanisms of electrolyte reabsorption, directly increasing the excretion of sodium and chloride. Indirectly, the diuretic action of hydrochlorothiazide reduces plasma volume, leading to increased plasma renin activity, aldosterone secretion, urinary potassium loss, and decreased serum potassium. The renin-aldosterone link is mediated by angiotensin II, so coadministration of an angiotensin II receptor antagonist (Losartan) helps reverse the potassium loss associated with thiazide diuretics.
Hypertension
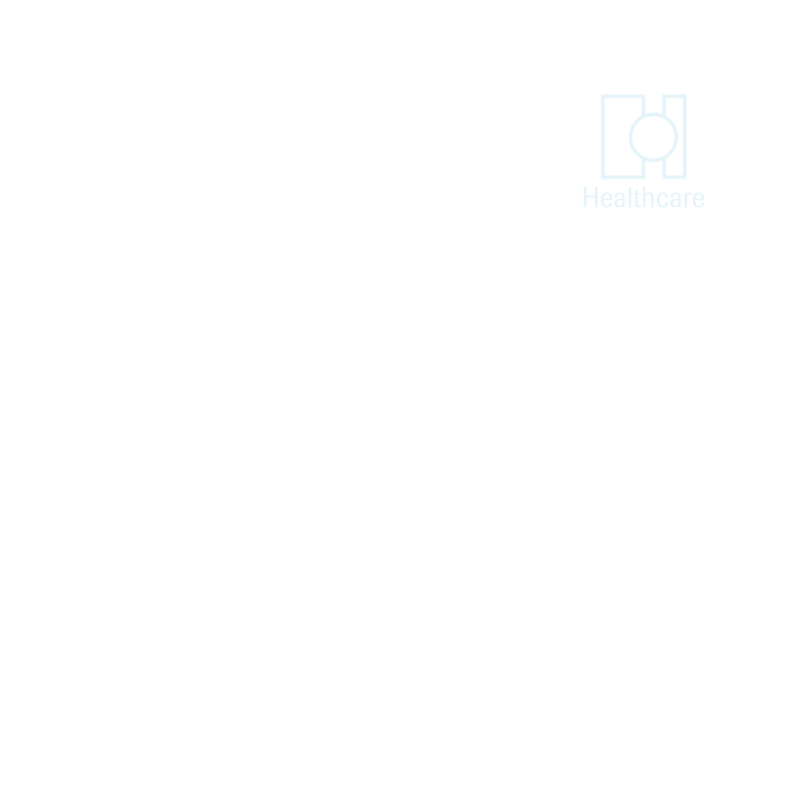
The usual starting dose of losartan is 50 mg once daily.
A lower dose of 25 mg is recommended for patients with intravascular volume depletion (e.g., patients treated with diuretics) and those with hepatic impairment.
The total daily dose can range from 25 to 100 mg.
Hydrochlorothiazide is effective at doses of 12.5 to 50 mg once daily and is available in Losacor® Plus (12.5 mg hydrochlorothiazide).
To minimize dose-dependent side effects, combination therapy is typically initiated only after a patient has failed to achieve the desired effect with monotherapy.
Hypertensive Patients with Left Ventricular Hypertrophy
Treatment should be initiated with losartan 50 mg once daily.
If blood pressure reduction is inadequate, hydrochlorothiazide 12.5 mg should be added.
Additional antihypertensives may be added for further blood pressure reduction if needed.

Losacor® and Losacor® Plus are contraindicated in patients who are hypersensitive to any component of this product. Due to the hydrochlorothiazide component, this product is also contraindicated in patients with anuria or hypersensitivity to other sulfonamide-derived drugs.
Losartan and losartan potassium-hydrochlorothiazide are generally well tolerated. Most adverse reactions are mild and transient and do not require discontinuation of therapy. The overall incidence of adverse effects is comparable to that of placebo. Some commonly reported adverse effects include:
Dizziness
Fatigue
Cough
Diarrhea
Pediatric: The pharmacokinetics of losartan has not been investigated in patients under 18 years of age.
Geriatric and Gender Differences: Elderly patients (65-75 years) and young hypertensives have similar plasma concentrations of losartan and its active metabolite.
Plasma concentrations of losartan were about twice as high in female hypertensives compared to male hypertensives, but the active metabolite concentrations were similar in both genders.

Renal Insufficiency: Renal function changes have been reported in susceptible individuals treated with losartan. These changes are reversible upon discontinuation.
In patients whose renal function depends on the renin-angiotensin-aldosterone system (e.g., severe congestive heart failure), treatment with angiotensin-converting enzyme (ACE) inhibitors has been associated with oliguria, progressive azotemia, and rarely, acute renal failure. Thiazides should be used cautiously in patients with severe renal disease due to the risk of azotemia.
Hepatic Insufficiency: Plasma concentrations of losartan and its active metabolite are significantly increased in cirrhotic patients.A lower dose should be considered for patients with hepatic impairment.
Losartan should not be used during pregnancy. If pregnancy is detected, the medication should be discontinued immediately.
It is unknown whether losartan is excreted in human milk, but thiazides are known to be present in breast milk.

Rifampin decreases losartan concentrations.
Ketoconazole does not affect the metabolism of losartan.
No clinically significant interactions were found with hydrochlorothiazide, digoxin, warfarin, cimetidine, or phenobarbital.